The lung secret code: who will survive? When bronchoscopy is not possible
PLAYERS
The patient The Oncologist
The Pulmonologist
Clinical case
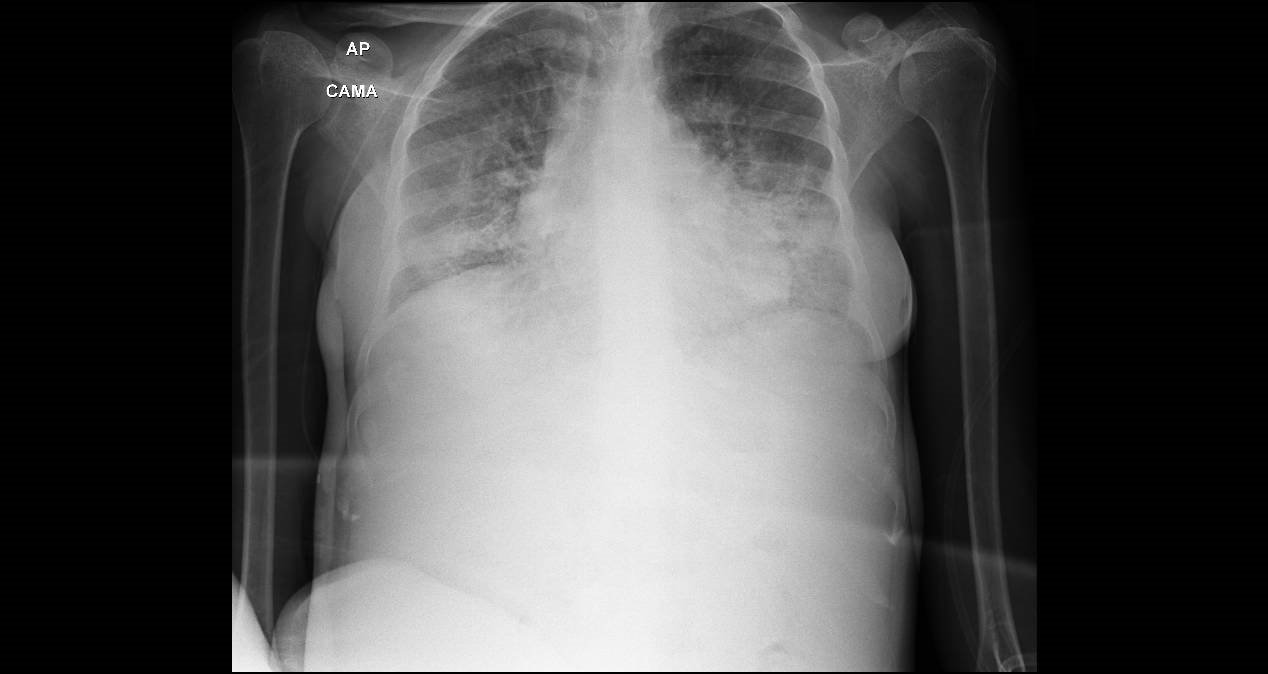
A 42-year-old woman had a diagnosis of metastatic breast cancer. She started treatment with chemotherapy, but ten days after her first cycle she went to the Emergency Department with symptoms of dyspnea, a non-productive cough and fever. Her blood test showed a normal hemoglobin, platelets and white cell count.The x-ray showed a bilateral alveolar pattern with a dramatic change in comparison with a normal x-ray a week before. The patient was treated with broad spectrum antibiotics (meropenem, vancomicin), trimethoprim sulfamethoxazole and metil-prednisolone.


Blood and urinary cultures were negative. Legionella and Pneumococcus antigenuria was not present . It was not possible to obtain a sample for a sputum culture.
The patient
“I can´t breathe, even when I move slowly my heart starts to beat fast and there is no air in my lungs, but on the other side I don´t have fever”. I was happy because the ulcer in my breast was improving with the chemotherapy.
The Oncologist
“I am quite sure that the patient has a pulmonary infection. The symptoms started in an acute way, and the images are associated with a widespread consolidation in both lungs. Of course I have discarded a pulmonary embolus as a worst-case scenario, but the Computer Tomography (CT) is normal in that aspect. I find surprising that the blood and urinary cultures are negative. Also the panel of antibodies for other atypical infections are negative, only there is only one positive borderline result for Chlamydia pneumofila. Should I pay attention to this positive test for Chlamydia? I do not think so.
I would like to obtain a histological sample, I will comment with the pulmonologist”.
The Pulmonologist
“Definitely, it would be very interesting to get a pulmonary sample trough a bronchoscopy, but the patient has a severe respiratory insufficiency and she is not going to be able to cope with the procedure”.
Clinical evolution
The patient finished a two week course of antibiotics with a mild respiratory improvement day by day, but very slowly. She was supported by a positive pressure device , high dose of steroids, morphine and a prophylactic dose of trimethoprim sulfamethoxazole.
We show here the last x-ray
Clinical reasoning aspects
There are some points worth considering in this not-so-unusual clinical situation:
- The first action with a patient with a severe respiratory insufficiency is safety. To achieve this objective, we have to maintain her oxygen saturation at least over 90%, then the proper oxygen concentration is mandatory. At the same time if we think in an infection, but we don´t know the etiology, we have to start a broad spectrum antibiotic combination, covering Gram negative and positive bacterias.
- Never forget the concept of “worst-case scenario” or the situations that you can´t miss. In this case we thought in a pulmonary embolus, based in the acute presentation and the severe respiratory insufficiency and the previous diagnosis of neoplasia.
- Always think in a common clinical situations that could share a similar radiographic pattern , for instance, cardiac failure, even in a young person.
- Evaluate if the patient could have a particular problem or exposure that it could be related to the actual clinical problem. In this case we thought that the patient could be immunodepressed, but she just started the chemotherapy treatment. She had not received steroids before. Her right breast was covered with a bandage because of the ulcer and then we realized that we have not obtained a sample from the breast.
- Take in consideration, even the smallest details, never left an information without a proper evaluation. In our case we wanted to look for more information about the bacteria Chlamydia pneumoniae. We learnt that the information about this type of pneumonia is scarce , but in several diagnostic resources are listed in a third position in the pool of atypical pneumonia. We have learned about subtle differences between Mycoplasma and Chlamydia pneumonia (1)
- When you suspect an infection and all the cultures are negative, it could be mandatory to obtain a histopathological sample. In the case of an organ like the lungs , bronchoscopy is the usual first diagnostic tool, followed by mediastinoscopy, thoracoscopy or video thoracoscopy. But, in this case, the patient had a severe respiratory insufficiency and it was impossible to get a bronchial sample.
- The response to treatment is also an orientation to confirm or not your diagnosis, at least established as a syndrome. If you see a clinical improvement with the treatment implemented, then you will feel more confident about your clinical reasoning process.
Final conclusion
The clinical evolution of the patient was positive. Although we were aware of the serological data, we thought that the finding could be a false positive for Chlamydia and we never confirm it with a PCR (Polymerase chain reaction).
We focused in the lungs, but you have to consider another possibles origins of the infection.
A detailed daily clinical evaluation is a key step to keep your patient safe.
The Oncologist
“Next time I have to look to every small detail, even if it is covered by a surgical bandage”.
Bibliography




