Everything is Written in Books, but you have to choose: Wernicke, Hypothyroidism? Or both?
Clinical Summary
We introduced here the clinical case of a-50-year-old male patient with a diagnosis of an epithelial cavum carcinoma, diagnosed eight months ago. He quit smoking thirteen years ago, and he was an occasional alcohol drinker. He has not other previous diseases. He underwent a combination of chemotherapy and radiotherapy seven months ago, and he has successfully completed his tumor treatment. He experienced side effects, such as an important impairment in swallowing and a weight loss of over 20 Kilogram, however, his appearance was not malnourished (he had previously weighed 100 kg). The radiotherapy field reached the mid-central region of the brain. He had, also, mucosal toxicity, and eating only liquid food in the last three months.
Clinical evolution
The family brought the patient to the Emergency Department (ED) during the weekend, because he started with a confusion and disorientation and difficulty to walk properly. The physical examination showed a confused patient. He was able to speak and to move his arm and legs, but he couldn´t stand up or to walk without help. A bilateral horizontal nystagmus was detected. A blood test, kidney function and serum levels of different elements, included calcium was normal. A CT scan without contrast was considered normal, without evidence of metastases or a major intracranial bleeding. He was admitted to the hospital on Friday.
The first possible diagnosis was neurological toxicity after radiotherapy over cavum and the brainstem.
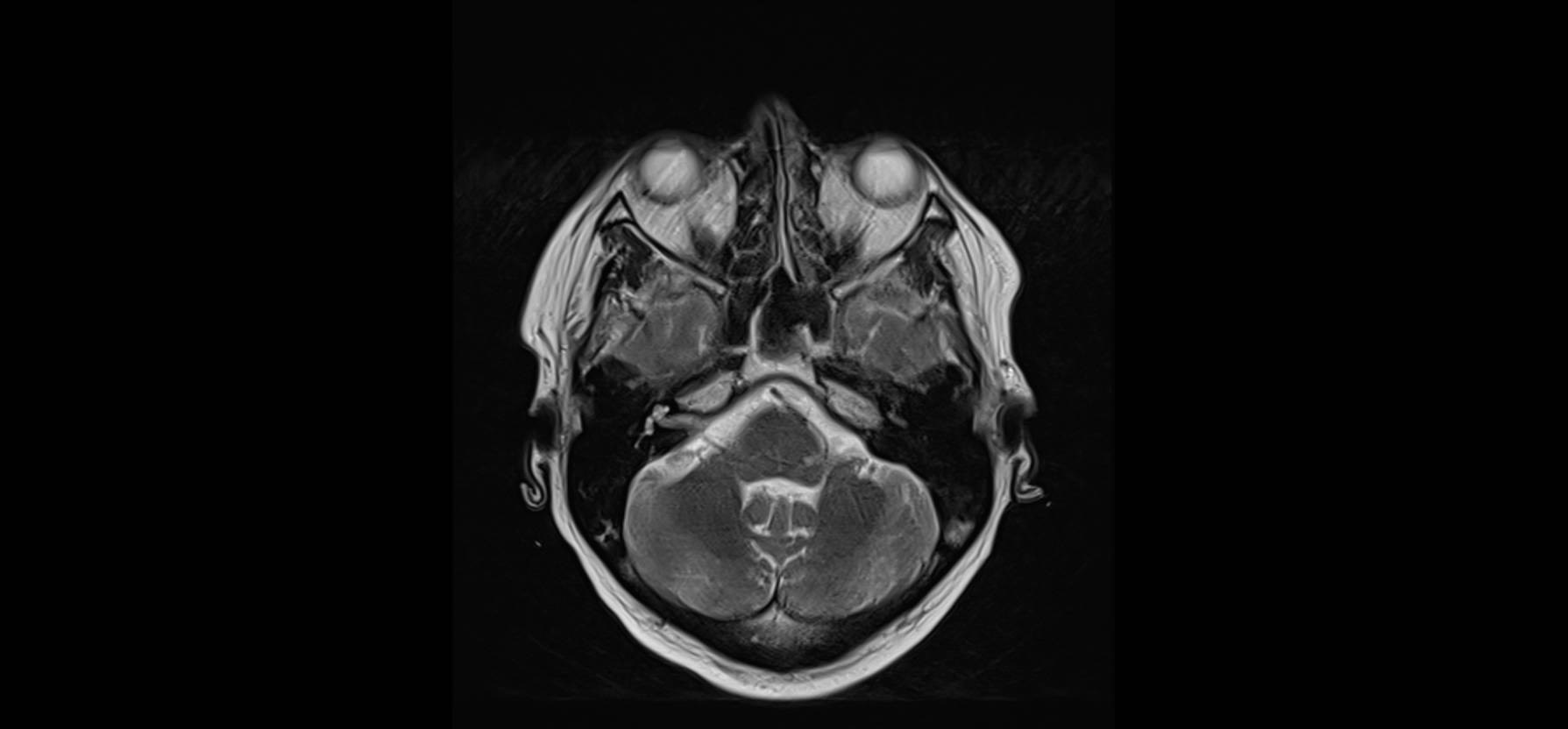
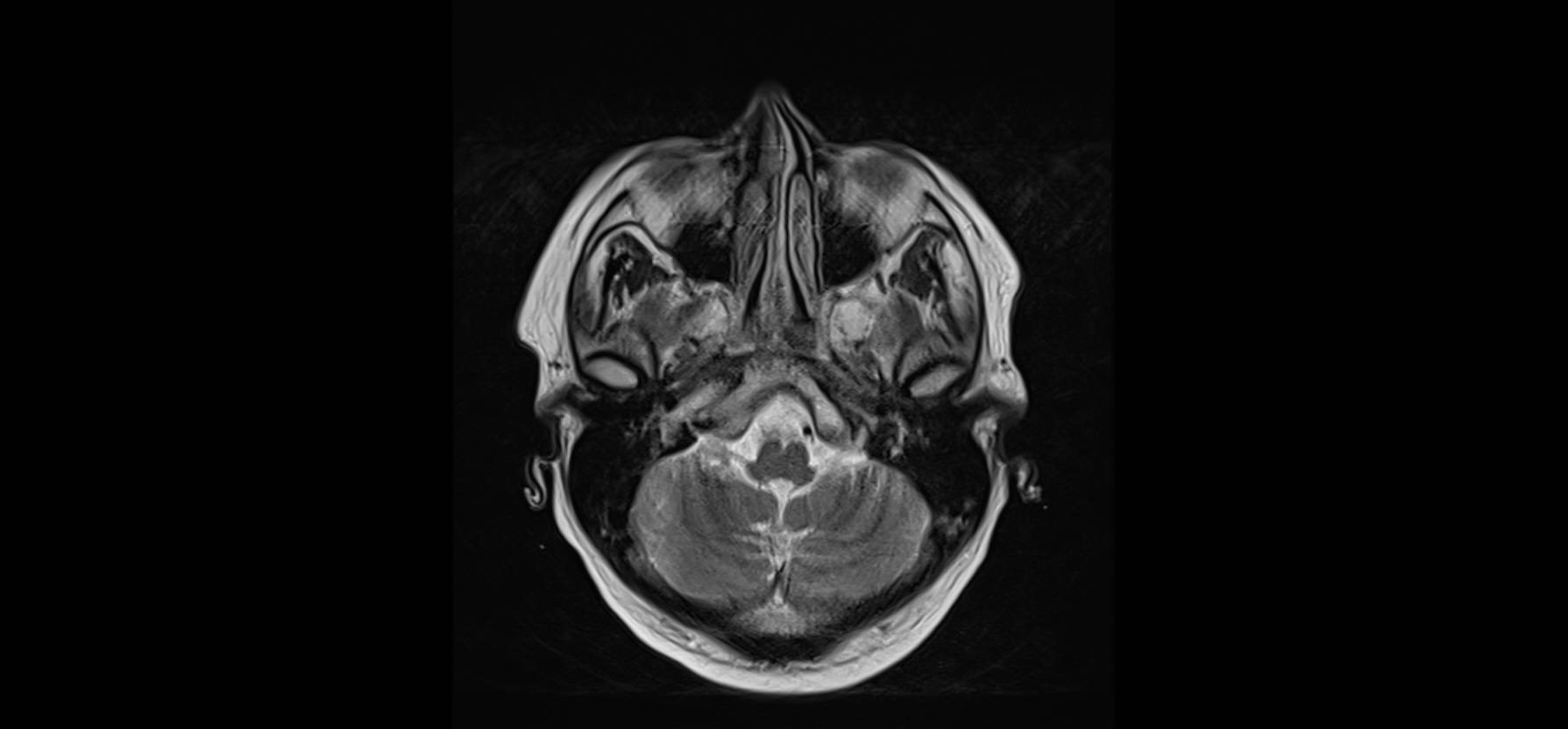
On Monday the physician in charge of the patient found him with confusion, disorientated, with the same problem with standing up, and with a bilateral and horizontal nystagmus. He asked for a Magnetic Resonance with contrast, and a selection of images are shown here
Patient follow-up
The patient started treatment with thiamine, steroids and intravenous fluids, and he was feeding through a nasogastric tube. The principal diagnosis, based on the clinical picture and the radiology, was Wernicke encephalopathy (WE), in relation to a lack of nutrients and vitamins, due to mucosal toxicity in the superior digestive tract.
A second battery of laboratory tests showed a high vitamine B12 level and a normal vitamine B1 level. There was a central hypothyroidism, with a low value for TSH, T3 and T4, and levothyroxin was administered to the patient.
After several days of treatment with thiamine and levothyroxine, the clinical situation of the patient improved, but without a complete normalization of the mental status.
Final Diagnoses
- Wernicke encephalopathy, due to a lack of a proper nutrition associated with mucosal toxicity after Radiotherapy (confusion, ataxia, nystagmus)
- Central hypothyroidism
Comment
This clinical case shows the complexity to reach a diagnosis in Clinical Medicine. Combining the clinical picture with the opinion of the radiologist, favours the choice of Wernicke’s encephalopathy as the most likely diagnosis. However, this case is also an example of the need to develop a complete differential diagnosis in clinical practice.
In the end, if we only consider a radiological image, we must think that, even if it is characteristic of a certain pathological process, other entities may be involved in the patient’s clinical picture (1), as it is the case exposed here. Medicine is not mathematics, and sometimes, when you expect a particular laboratory finding, for instance a low thiamine value in the blood, you see a normal value, like in the present patient. Usually, this situation can be explained because there are several metabolic pathways in the same direction, as a chain. WE is primarily a clinical diagnosis, and laboratory and radiology help in this diagnosis.
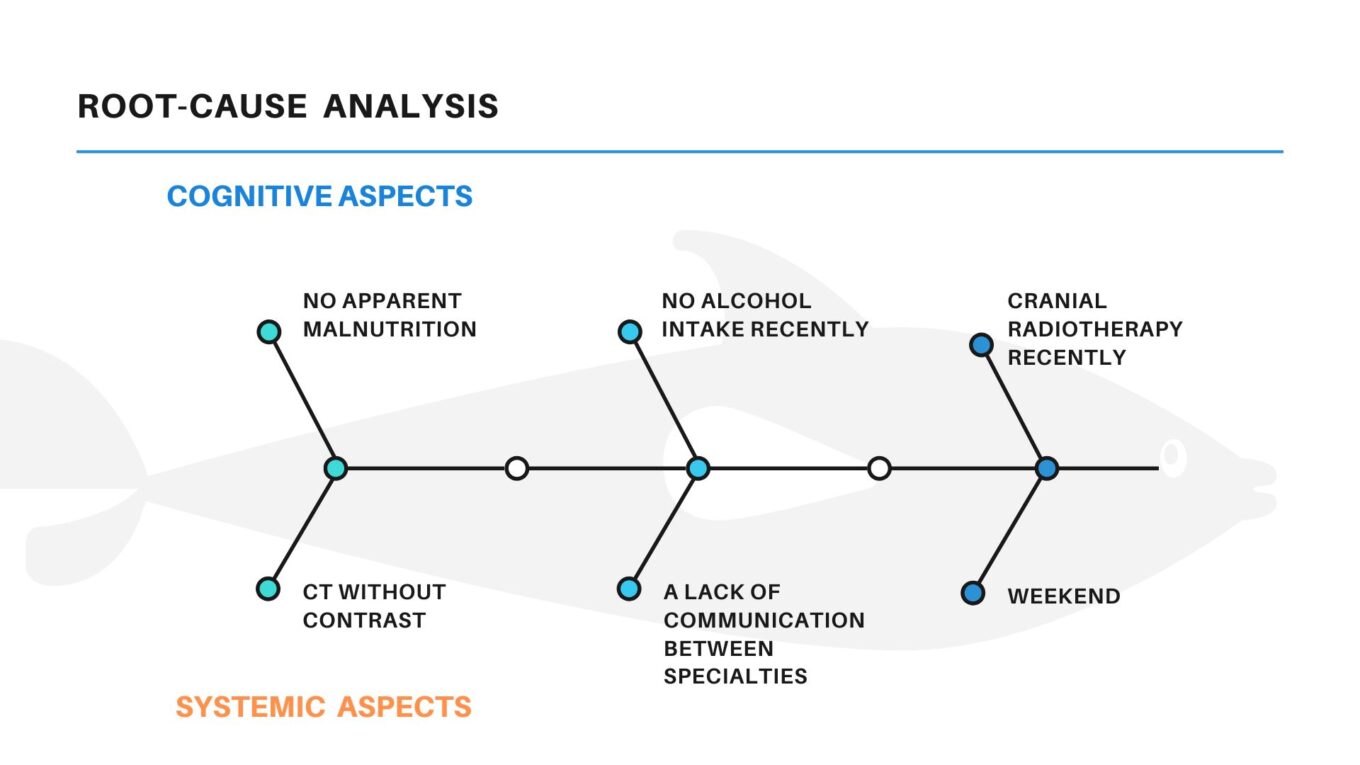
Analysis
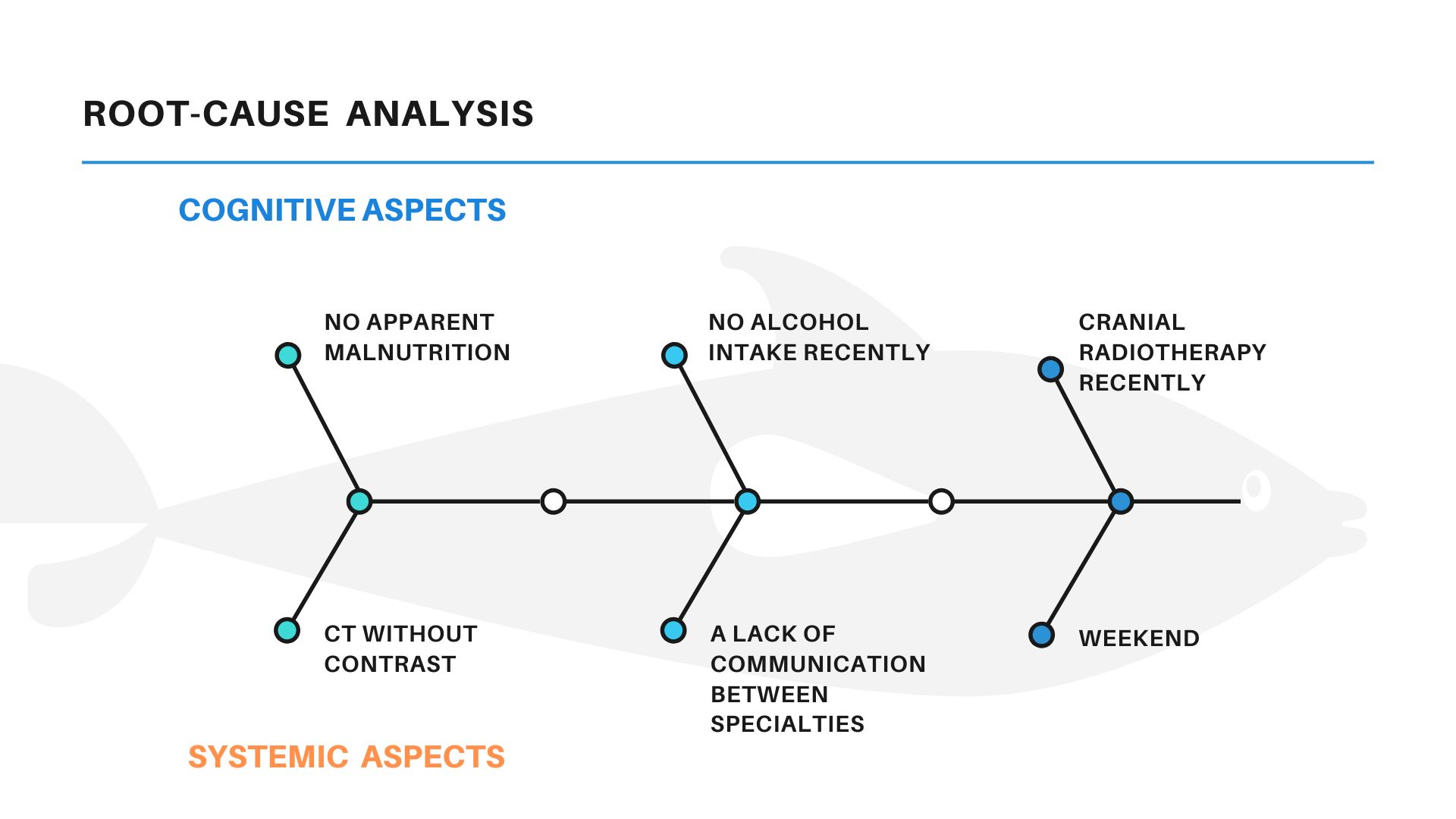
The question here is: If Wernicke encephalopathy is a “worst-case scenario”, in a situation of confusion, ataxia and nystagmus, in the proper context of a patient with a poor nutritional situation, Why was not considered initially in the complex world of the Emergency Department?
We show here a Root-cause analysis, with some cognitive and systemic factors, that we consider can help to explain this situation, at least partially.
Bibliography
1)Wernicke encephalopathy: MR findings at clinical presentation in twenty-six alcoholic and nonalcoholic patients. AJNR Am J Neuroradiol2007 Aug;28(7):1328-31.
Author: Dr. Lorenzo Alonso Carrión
FORO OSLER