Karma and The Disease. Learning from Patients in Clinical Medicine
Introduction
She was in bed, a 55-year-old woman, unable to move her legs and arms, absolutely depending of people. She could speak and even to take some food with the help of her family. I was there, standing up close to her, a senior doctor asking questions about her feelings and symptoms. In a moment she asked me. “Do you know what karma is? “. I got a little bit surprised, I remembered the word, many times I had read about it, but at that particular moment I couldn´t answer to her. She explained to me: “Karma is a movement, everything is connected, when you are giving a person something good or love, you will receive also love in some moment during your life”.
Case Summary
A-55-year old woman had a previous diagnosis of a uterine sarcoma six years before the present clinical situation. She was treated initially with surgery and adjuvant Radiotherapy, but the disease disseminated to the abdomen and lungs, starting treatment in a sequential way with chemotherapy and target drugs, reaching a complete response in the last clinical follow-up.
Clinical Evolution
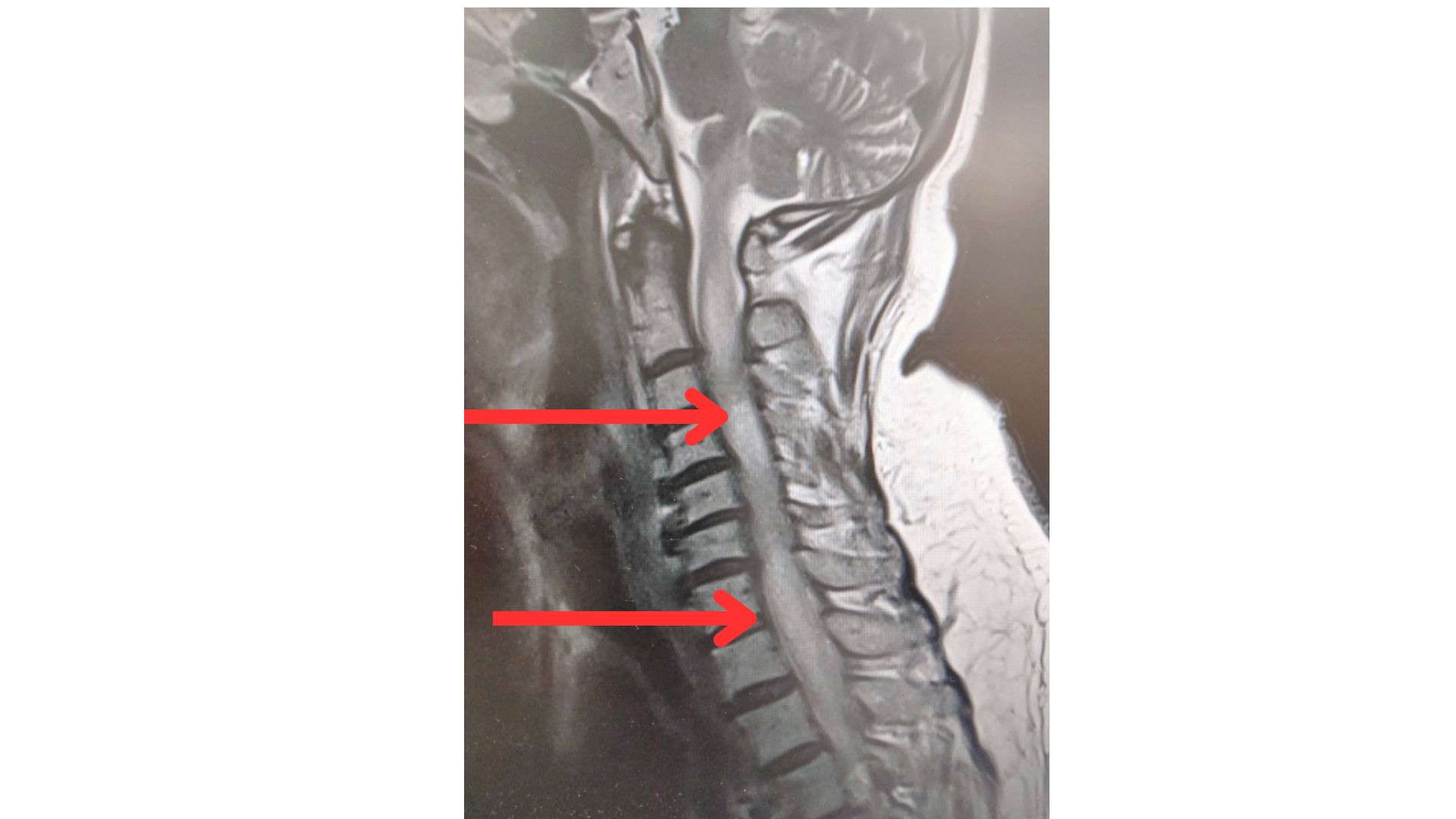
She went to the Emergency Department (ED) because, after a fall, she started with a progressive difficulty to move her legs, reaching to a total paralysis, and progressing upward to both arms, until a situation of tetraplegia in a two-day period, preserving the ability to speak and to swallow, with a normal mental status, without fever or back pain.
The physical examination showed an alert patient, totally orientated, with no respiratory compromise. There was a flaccid paralysis of all four extremities, and a mid-dorsal sensory level. No extensor plantar response was present. A urinary catheter had to be placed due to urinary retention.
Clinical Reasoning Exercise. Situation Awareness
Imagine now that you are in the ED in your first contact with this patient. Remember that she had a previous diagnosis of a neoplastic disease. With the clinical picture exposed previously, What would be your first diagnostic possibility?
- It is clear that the presence of a paraplegia in a patient with a diagnosis of cancer will trigger the possibility of a spinal cord compression. In a way, this is the “worst-case scenario” diagnosis, in a clinical situation like the one we have just described. However, there are some cues that can be helpful for a more accurate decision, and to fit a better clinical model.
- Back pain. In a spinal cord compression, the presence of back pain as an initial and early symptom is almost universal. In the case exposed, the patient never referred back pain in the days preceding the actual clinical situation.
- No pyramidal symptoms. In the early phase of a spinal cord compression, there is hyperreflexia below the level of the compression, a data lacking in the physical examination of our patient.
A doctor in charge of the patient will think initially in a spinal cord compression, but after a quick reasoning process, he or she will be aware of the different presentation of the tetraplegia of this patient, without pain preceding the paraplegia and the situation of a flaccid paralysis, without a previous period of hyperreflexia in relation with the interruption of the pyramidal pathway. When the clinical model doesn´t fit an important sign or symptom, it is mandatory to broad the differential diagnosis. The first step is the anatomic location of the problem, in this case the spinal cord or the vertebral structure.
Final Comment
The patient was unable to move their arms and legs, but she always kept her mind under control. Lumbar puncture was not performed. No clinical response to steroid treatment was observed. The final clinical diagnosis was a medullary infiltration of the tumor from T2 to T7, with edema along the rest of the spinal cord.
It is important for a physician to do always the mental exercise of a differential diagnosis, maybe in a particular case the clinical attitude or treatment will not change too much, but, at the end, you will be more expert in the next clinical case or patient, and, for sure, this is the path to reach expertise in Medicine o Nursing.
You will find a good review about spinal metastases in general in the paper HERE
Author: Dr. Lorenzo Alonso Carrión
FORO OSLER


