What we don’t know is more than we know. Learning new clinical environment from new drugs
Objective
The knowledge transmited to medical students in medical schools is exposed in “positive” terms, describing a bunch of diseases with a clear constellations of signs and symptoms, but clinical practice is more an exercise of disantangle and exclusion than an afirmation.
Fever, a sign with multiple faces
A-62-year old man had a diagnosis of kidney cancer with lung metastases. He was receiving treatment with Nivolumab, a drug directed to increase the immune response against the tumor.
He started acutely with a high fever(38,5 centigrades), without respiratory, digestive or urinary symptoms. He has had two previous episodes in the last three monts with fever, an increase in liver enzymes, mild increase in the direct bilirrubin value and a prolonged protrombine time, recovering totally with steroids and antibiotics.
The current physical examination showed a patient with fever, lethargy and a low blood pressure (BP 90/50 cm).
Laboratory: Blood test showed leukopenia (1100 mm3) and thrombocytopenia (45.000 mcL), with an increase in the PCR value (146 mg/l, normal value less of 4 mg/l) and the procalcitonin level(6 ng/ml, normal range less of 0.5 ng/ml). The liver enzymes were three times over its normal value, a 60% prothrombin time and a direct bilirrubin value in the superior limit of a normal range(1,5 mg).
Two blood cultures were positive for a Gram+ bacteria ( Mycrococcus luteus).
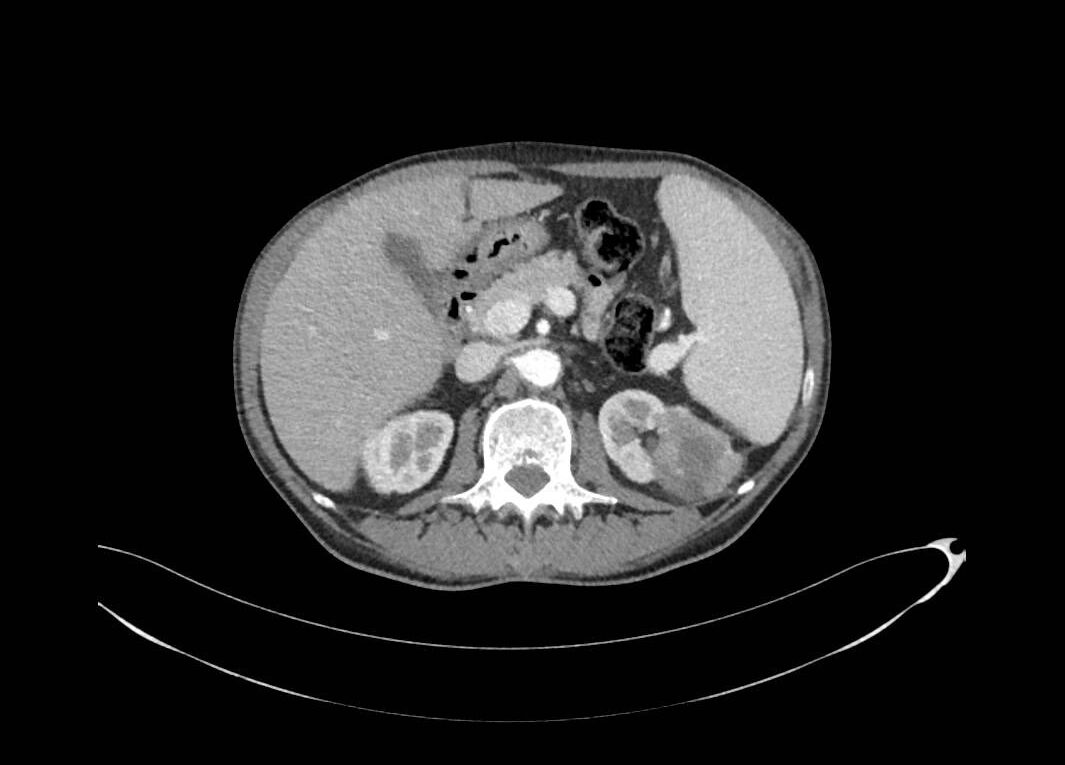
A liver sonogram and an abdominal CT scan showed an increase in the size of the liver and the spleen, with a high venous portal pressure, and intrahepatic cholestasis, but no metastases.

A summary report
We have here the clinical case of a middle age man, with a diagnosis of metastatic kidney cancer to the lung, treated with an immunostimulant agent, with fever, a positive blood culture, analytical data of “inflamation”(increase in Protein C Reactive, procalcitonin) and data of liver damage with a high transaminases value.
Question 1
We want you to select one of three possible pathways, but we are going to help you narrowing the possibilities:
- Sepsis with bacteriemia and liver damage, then treat with antibiotics
- Liver toxicity (hepatitis autoimmune) associated with Nivolumab, then treat with steroids
- Sepsis plus hepatitis autoimmune
- We are going to give you the option of a fourth possibility, after you will read this paper: here Stauffer’s Syndrome Variant with Cholestatic Jaundice A Case Report
Question 2
Can you find a key data to differentiate between a Stauffer´s Syndrome and a possible hepatitis autoimmune?
Please make your comments in this page. Thank you
Author:Dr. Lorenzo Alonso Carrión. Medical Oncology
FORO OSLER



I was not familiar with this syndrome. It was a great learning experience about anicteric cholestasis. Autoimmune drug-induced liver injury (DILI-ALH) and adverse effects are complications that we always need to be vigilant about with new medications.
(https://www.journal-of-hepatology.eu/article/S0168-8278(23)00320-3/fulltext) (https://www.ncbi.nlm.nih.gov/books/NBK548206/ )
Thanks for sharing.