Sepsis and the System: a Better Equipment Improves the Diagnostic Process
Sepsis and the System: a Better Equipment Improves the Diagnostic Process
When a doctor visit a patient with a combination of high fever, chills and low blood pressure, he or she knows that the patient is in danger, under the effect of an infection, and in this situation the sooner the better for the identification of the bacteria and to start the specific antibiotic.
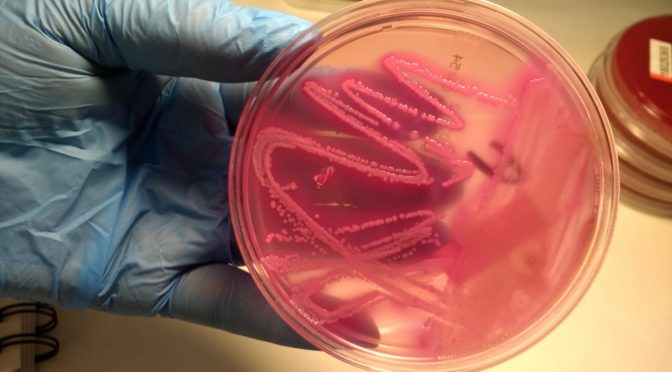
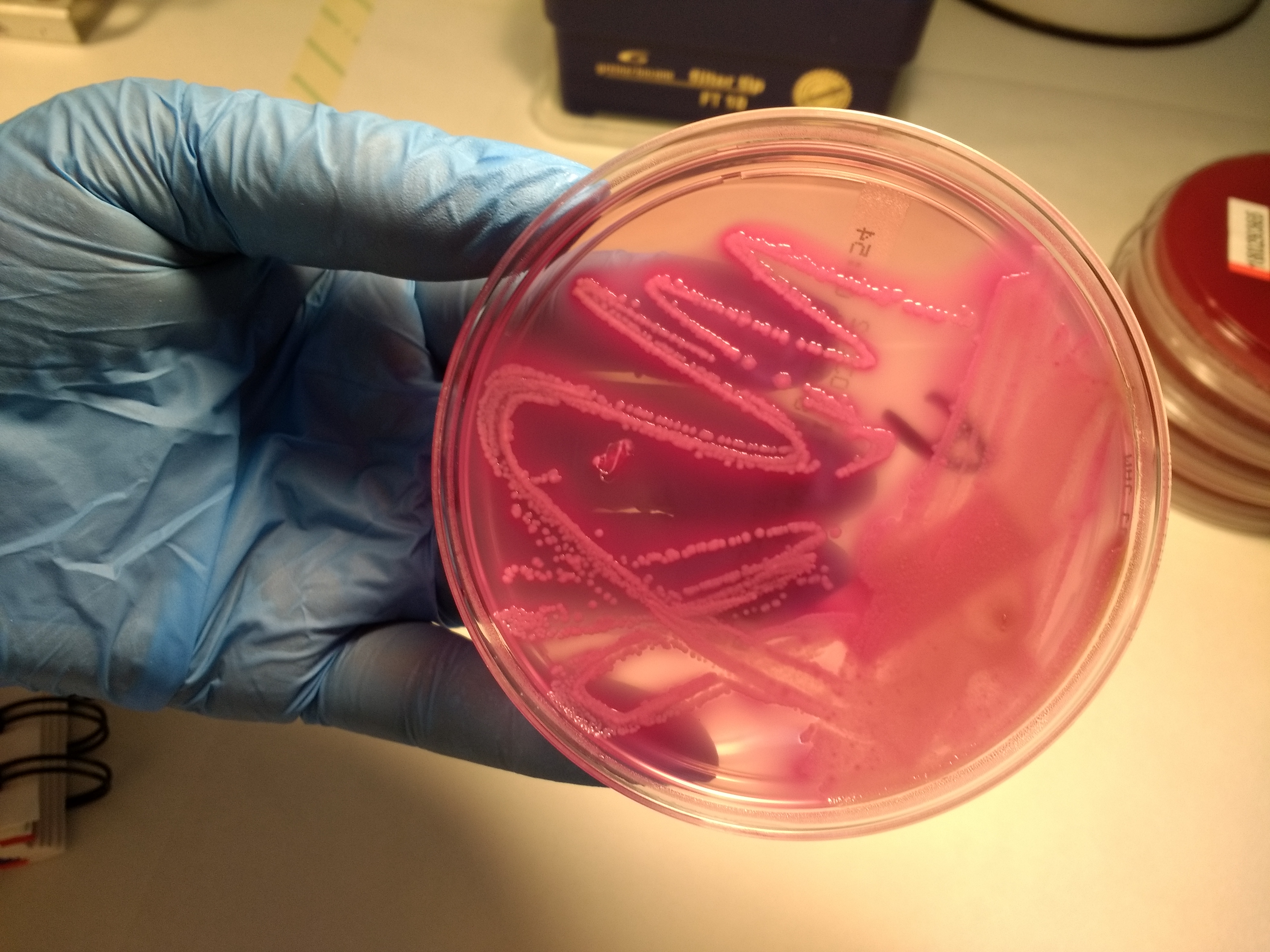
Not too long ago the procedure to identify the bacteria included to put the sample in a culture medium, to wait to see some bacterial growth, and then to use an optical microscope to give the final diagnosis. Usually this procedure, in the best of the situations, lasted for 3 to 5 days, a period of time where a doctor was not able to start with the specific antibacterial drug.
What do we have now?
The microbiology lab is a key area in a hospital, and every change have a direct impact on clinical practice, for a faster diagnosis or for a better treatment. In many labs the optical identification has been replaced for more sophisticated techniques based on multiple genetic identification, thanks to automatic machines. Now, in less than 24 hours a doctor can get the exact bacteria causing the infection and to start the specific drug. This is a clear example of the permanent interaction between the “System” and the diagnostic process.

What are the implications for clinical practice?
First, once we know the exact bacteria inside the bloodstream of the patient, the doctor can select the treatment, usually reducing the number of antibiotics to just one, the specific for the patient, because during the diagnosis period several antibiotics must be used to “cover” all the possible etiologic agents. Second, the patient´s safety is increased, through a reduction in the period of time needed to detect the bacteria and to treat the patient. Moreover, there is a reduction of the probability of an adverse event, because antibiotics have a broad panel of toxic effects.