“My legs are very weak and my back hurts so much”
“My legs are very weak and my back hurst so much”
Author: Lorenzo Alonso
FORO OSLER
Clinical summary
A 57-years-old-man had a diagnosis of kidney cancer with bone metastases including the spine. He was receiving treatment with immunotherapy. One week before the hospital consultation, he started with back pain, walking difficulties, a feeling of weakness in both legs, with difficulty in urination. He has had no feverThe general physical examination was normal. The neurologic examination showed a significative weakness on his legs, with an impossibility to walk and to stand-up from a chair. Patellar reflexes were exacerbated. There was a clearly sensory thoracic level, reaching until the inguinal region. A urinary catheter had to be inserted due to a bladder retention.
The blood test was normal. A lumbar puncture showed an increase in the protein and white cell levels and a normal glucose value.
A plain X-ray from the spine showed some lytic lesions, but no vertebral destruction.
An MRI was scheduled.
SITUATIONAL REASONING

A) EMERGENCY DEPARTMENT (ED):
Probably if you were a doctor in the ED your first thought about the problem of this patient will be a clinical picture associated with his diagnosis of a metastatic kidney cancer. The important symptoms here are back pain and the weakness in the legs. Thinking under the strategy of a “worst-case scenario”, a spinal cord compression must be discarded.
B) GENERAL PRACTITIONER (GP):
A General Practitioner (GP) working in a Health Center, without an accessible diagnostic tool such as a CT or an X-ray, will be under professional stress in this type of situations. Moreover, time is scarce in these facilities, due to the high number of people that usually wait every day to be attended by the same doctor. In this scenario will be very difficult to examine a patient and, even more, to look for specific details like a sensory level or the ability to walk. Maybe the GP will think about metastases, or a discal hernia or in the worst-case scenario he or she will think in a spinal cord compression, referring the patient to the hospital. Probably he or she would start a treatment with a painkiller and scheduled a new visit in a short period of time.
C) INTERNIST AND MEDICAL ONCOLOGIST
Immunotherapy is now widespread in the treatment of patients with cancer. There are important and uncommon side effects specific of this treatment, the majority of them associated with the possibility of an autoimmune response targeting every single organ and structure in the body. Internist and medical oncologist working together are now accustomed to detect these side effects that mimic a wide range of pathological entities. For this reason, the immune related side effects must be included in the differential.
DIFFERENTIAL DIAGNOSIS
The differential included three possible diagnoses:
- Spinal cord compression
- Guillain- Barré syndrome
- Transverse myelitis immune related
EVOLUTION OF THE STORY
The MRI report discarded a spinal cord compression. During the first days of his stay at the hospital, doctors were not sure about the diagnosis. The patient was treated with steroids (prednisone 1mg/per Kg. weight), with an improvement in the back pain. After two weeks the patient was able to stand-up from the chair and to walk with a little help.
FINAL DIAGNOSIS
.Transverse myelitis, immunorelated
KEY DIFFERENTIATE POINTS
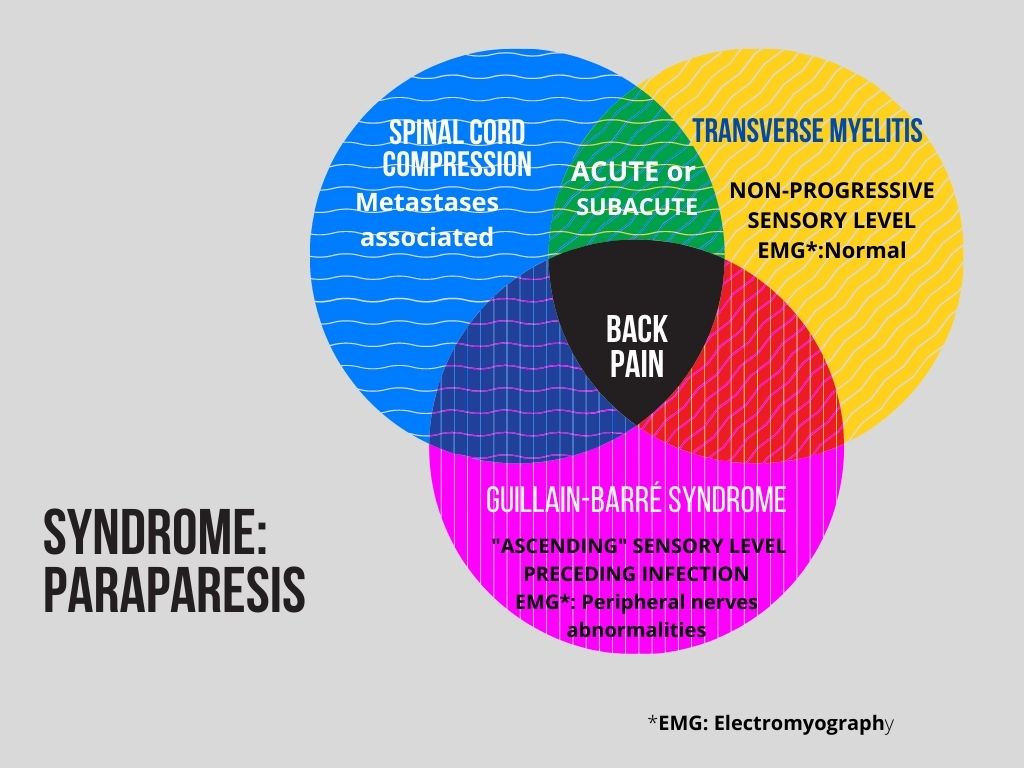
There are some key aspects to differentiate between entities. The spinal cord compression must be confirmed or not with the MRI. The clinical picture can be similar initially for the transverse myelitis and the Guillain-Barré syndrome, but after a more complete approach it is not difficult to differentiate among them. In the Guillain-Barré syndrome, there is usually an “ascending” motor deficit, going for the legs to the arms, what is not seen in the Transverse myelitis. There are other differentiating factors that you could see here



