Do you think it could have been done better? Abdominal pain, nausea and vomiting
Do you think it could have been done better? Abdominal pain, nausea and vomiting
The storyteller
A 50-year-old woman without previous diseases went to the Emergency Department (ED) because in the last week she started with pain in her abdomen and vomiting after eating. She was a heavy smoker with two episodes of right ureteral lithiasis four years ago.
She had four consultations for the same problem, the first one with her General Practitioner and the rest in the Emergency Department (ED), all of them in a period of one month and a half.
The patient (after the definitive diagnosis)
“I was feeling pain and I couldn´t eat, I was not hungry, but the worst thing for me was the desperation because no one paid a proper medical attention to me. I had to go to a private doctor and he did an abdominal ultrasound and he made the diagnosis”. Blood tests and kidney function were normal. The first doctor advised me to follow a soft diet. In the other three visits to the ED , just one doctor spoke to me about my diagnosis: Epygastralgia,

Final Diagnosis: Gastric adenocarcinoma
How the diagnosis was made?
A private doctor decided to practice an abdominal ultrasound and he detected an abdominal lump and gastric dilatation. An endoscopy allowed to obtain a gastric biopsy.
Case Analysis
In summary, we have a previous healthy woman with a short period of clinical symptoms (around two months), some of them shared with several clinical entities. We need to answer to some questions before the analysis;
- Professional aspects: how was the anamnesis? The patient referred that she was not hungry for several days and she also referred vomiting every time she ate something. When enough clinical information was available at the first encounter with the patient a delayed diagnosis is considered a diagnostic error or “missed opportunities” (1). The symptoms referred by the patient in a “continuous base” could be framed inside this concept.
- The physical examination of the abdomen was normal, but this is a very subtle and soft data, because is based on the expertise and the time invested in it. We don,t know if a more orientated exam of the abdomen could be found more information
- There was also a false impression of “techtrust”, because a plain abdominal x-ray has a limited decision value in this context, at least with negative findings. However, the image showed here is, at least peculiar, worthy of more search.
- Number of visits: it is well known after the research by Lyratzopoulos (2) who suggested that the proportion of patients with a given cancer who experience multiple (e.g. three or more) primary care consultations before specialist referral could be considered as a marker of the difficulty of suspecting that cancer at first presentation. In the everyday clinic is not uncommon to see this situation, mainly in young people or for women for some specific locations.
Fishbone diagram
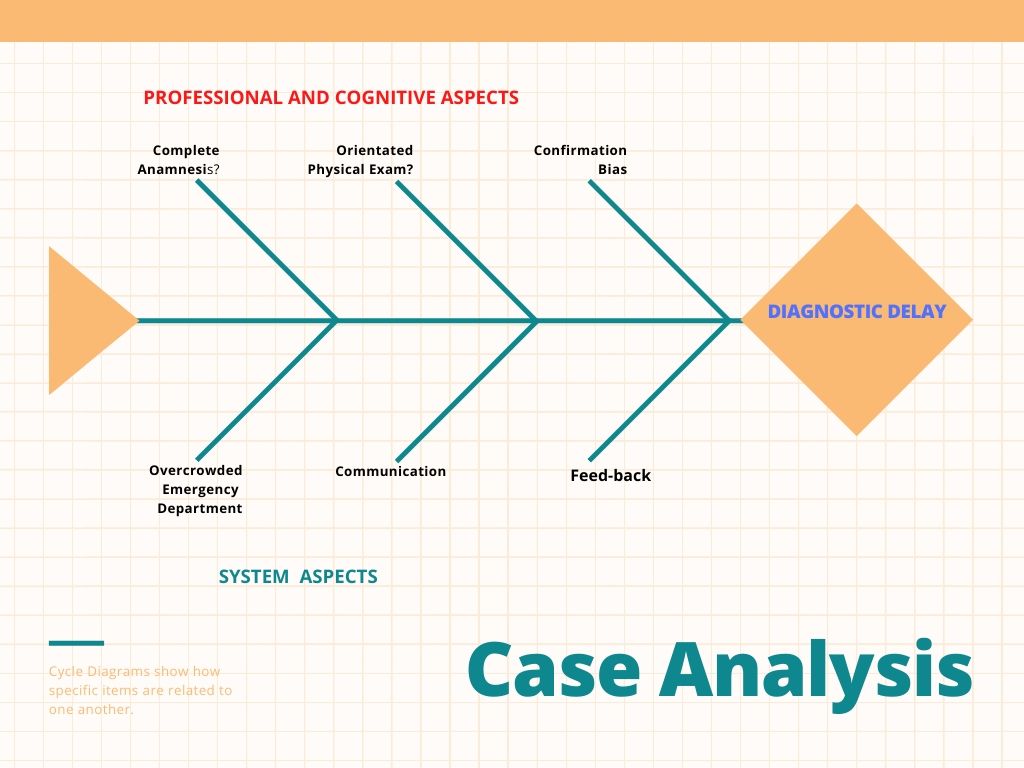
Cognitive aspects
If we could select one cognitive bias in the whole chain of clinical reasoning, we could say that every doctor was in a situation of “confirmation bias”, trying to confirm their thoughts that a young person without the “cachexia syndrome” can, t have a cancer.
System aspects
There was not a “safety net” organized for the patient, to do a follow-up to know the clinical evolution, and there was also a lack of effective communication between physicians.
Bibliography
- Singh H, Sethi S, Raber M, Petersen LA. Were my diagnosis and treatment correct? No news is not necessarily good news. J Gen Intern Med 2014; 29: 1087-1089
2. LyratzopoulosSingh H, Sethi S, Raber M, Petersen LA. Were my diagnosis and treatment correct? Rethinking diagnostic delay in cancer: how difficult is the diagnosis?. BMJ 2014; 349: 1-6
Author: Lorenzo Alonso, MD
FORO OSLER